Disabling Diseases in the Americas: The Promising Role of Peptides
- Antonio Carlos Faustino

- Jul 18
- 3 min read
Introduction
Disabling diseases in the Americas affect millions of people, causing loss of autonomy and quality of life. These are progressive, chronic, and often incurable diseases, such as Alzheimer's, Parkinson's, amyotrophic lateral sclerosis (ALS), and advanced diabetes.
In the Americas, population aging and the rise in metabolic diseases have increased the impact of these conditions. The demand for innovative , more effective therapies with fewer adverse effects has never been more urgent.
Research into peptides —small fragments of proteins with specific actions in the body—has been growing as they show potential to modulate inflammation, neuroprotection, and metabolism.
In this article, the reader will find an overview focused on what matters most: how recent research is opening real paths to treating debilitating diseases. From clinical challenges to advances in peptide trials, the reader will discover a connection between science, hope, and practical application.
Disabling Diseases in the Americas: A Current Overview
In the Americas, the most disabling are: Alzheimer's and other dementias , Parkinson's , ALS , type 2 diabetes and its complications , as well as serious cardiovascular and autoimmune diseases. These conditions cause dementia, motor loss, and incapacitation for basic tasks. This scenario demands effective treatments.
The social and economic impact of disabling diseases
These diseases increase social assistance costs, prolonged treatments, and time off work. Lost productivity and medical care costs jeopardize families and healthcare systems throughout Latin America and the United States, making new therapeutic approaches essential.
Peptides: what they are and how they work in the body
Peptides are short chains of amino acids that act as bioactive messengers in the body, regulating the immune system, inflammation, cell growth, and metabolic function. Many of them are already used as medications, such as insulin and GLP-1 agonists.
Recent research with peptides in the treatment of chronic diseases
Studies show that anti-inflammatory, immunomodulatory, and neuroprotective peptides can alleviate chronic pain, regulate metabolism, and protect neurons. In clinical trials, GLP-1 (such as semaglutide or liraglutide) demonstrate benefits not only in diabetes but also in systemic inflammation and neurodegenerative diseases.
Peptides and neurodegenerative diseases: promising advances
Bioactives such as NAP, ADNF-9, and Humanin have demonstrated, in animal models, protection against neuronal death and reduction of toxic aggregates related to Alzheimer's disease and ALS . Initial trials suggest neuroprotective effects, but with logistical and brain delivery limitations.
Furthermore, new therapies with incretin agonist peptides (GLP-1/GIP) have neuroinflammatory effects and are being tested in patients with Alzheimer's and Parkinson's disease, with promising results in phase II and III trials .
Use of peptides in muscle, joint and metabolic treatments
Peptides have potential in muscle recovery and in controlling obesity and diabetes. In type 2 diabetes, GLP-1 agonists help with glycemic control, weight loss, and may even reduce cardiovascular risk. New York Post . Studies in arthritis and chronic pain indicate that inflammation-modulating peptides (such as enkephalins and VIP) provide relief with fewer adverse effects than opioids.
Challenges and limitations in peptide research
Despite their potential, peptides face challenges such as poor stability, the need for injections, the blood-brain barrier, and the risk of immunological reactions. Few peptides have reached the clinical stage in humans, and long-term results are still scarce.
The Future of Therapeutic Peptide Use in the Americas
The growth in proteomic biomarkers of neurodegeneration and nanoparticle drug delivery (such as peptide-functionalized nanocarriers) offers new hope. A recent example: engineered nanoparticles with peptides that cross the brain barrier, improving symptoms in models of cachexia and central nervous system diseases.
In parallel, trials such as those with the monoclonal antibody prasinezumab (still in development, but derived from a peptide/anti-α-synuclein mechanism) are progressing in early Parkinson's and other compounds such as dihexa (potent neurotrophic) and LBT-3627 (dopaminergic immune modulator) are in preclinical studies .
Visuals, links, and multimedia
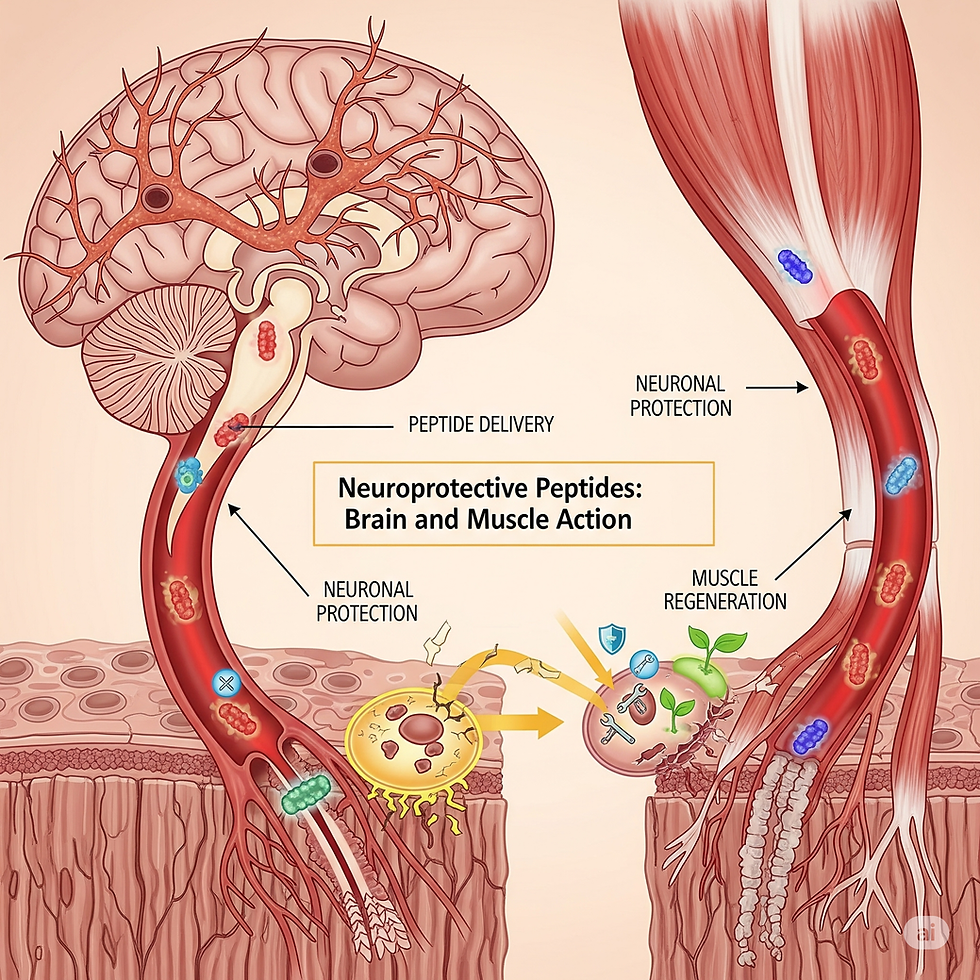
Image suggestion : Illustrative graph showing the action of neuroprotective peptides in the brain and muscle. Alt text : Diagram of neuroprotective peptides acting against degenerated neurons.
Short video : explaining how peptides cross the blood-brain barrier.
External links :
PubMed on neurotoxic peptides: https://pubmed.ncbi.nlm.nih.gov/34544337/
Cochrane for chronic therapies:
https://www.cochrane.org/pt/evidence/CD009790_exercise-treatment-chronic-low-back-pain .
Internal links :
https://www.bomdiaamericablog.com/post/expectativa-de-vida-nas-américas-desigualdades-e-desafios
Product recommendation (Amazon and Hotmart)
Amazon Products:
Hotmart Infoproducts:
Online course “ Peptides for health and longevity ”
References
SINGH, K. et al. A Review of the Common Neurodegenerative Disorders. Curr. Protein Pept. Sci. , 2024. PMC+4Wikipedia+4pubmed.ncbi.nlm.nih.gov+4 Wiley Online Library+3pubmed.ncbi.nlm.nih.gov+3pubmed.ncbi.nlm.nih.gov+3
LA MANNA, S. et al. Peptides as Therapeutic Agents for Inflammatory-Related Diseases. Int. J. Mol. Sci. , 2018. PMC+1pubmed.ncbi.nlm.nih.gov+1
CICERO, AF et al. Potential role of bioactive peptides in prevention and treatment of chronic diseases. Br. J. Pharmacol. , 2017. Wiley Online Library
VARIOUS PAPERS on GLP-1 agonists and neuroinflammation. FT, Time, NYPost , 2024-2025.




Comments